
Looking for a Way to Make Your Home Health Operations More Efficient? Here are Some Changes to Consider.
Home healthcare can be very rewarding. But I know it can also be very taxing at times.
So, let me ask you: what frustrates you most in your day? What keeps you from feeling totally fulfilled by your work? What would you change if you could?
Is it the effort it takes to gather all the necessary supplies and equipment to support your many different patients? The time on the road? The size of your case load?
Or do you find yourself struggling most to provide a high level of patient care when your technology tools aren’t working like they should (or you don’t have technology at all for certain tasks)?
For example, does your frustration stem from the spotty wireless connectivity that keeps you from retrieving or updating patients’ medical records while on the move? Or the fact that you don’t have a way to digitally access patient records from your mobile device, tablet or laptop, forcing you to pick up, refer to and update paper charts (which sets you up to make a whole host of mistakes)?
Are you just frustrated by how long it takes to document patient vitals because the medical devices you’re using don’t talk to the other devices – or your mobile device?
Maybe you’re having to visually confirm that you’re giving each patient the right dose of the right medication at the right time via the right method? Or call doctors to confirm the latest treatment plans, which could leave you sitting on hold – and sitting still – during busy days?
Perhaps it’s not a technology performance issue that makes your day harder, but the fact that you have too much technology to manage as a field-based worker (i.e., a laptop, tablet and mobile device). (Or that you have to manage technology at all.)
I’m sure when you signed up to be a clinician, you sought joy in a patient’s eyes as you gave them comfort and rehabilitation when they needed it most. You didn’t sign up to dedicate large portions of your time to secondary tasks like tracking down patient information and documentation, charting and troubleshooting tech, at the expense of your patient’s healthcare experience or your health.
So, what if I told you your day – and your entire job – could be easier?
Imagine this…
When you wake up, you quickly login to your large-screen (yet lightweight) tablet using single sign on (SSO) to access your schedule and inventory needs in one place. All your patients’ information is available from that same home screen, too – current treatment plans already verified with their physicians, the latest vitals and lab/radiology results in their records, and scheduling details spelled out (and accessible) in front of you. With no phone calls or other investigative work needed, you can ease into the day – enjoying your breakfast, working out, spending time with the family, or doing whatever it is you do to get energized.
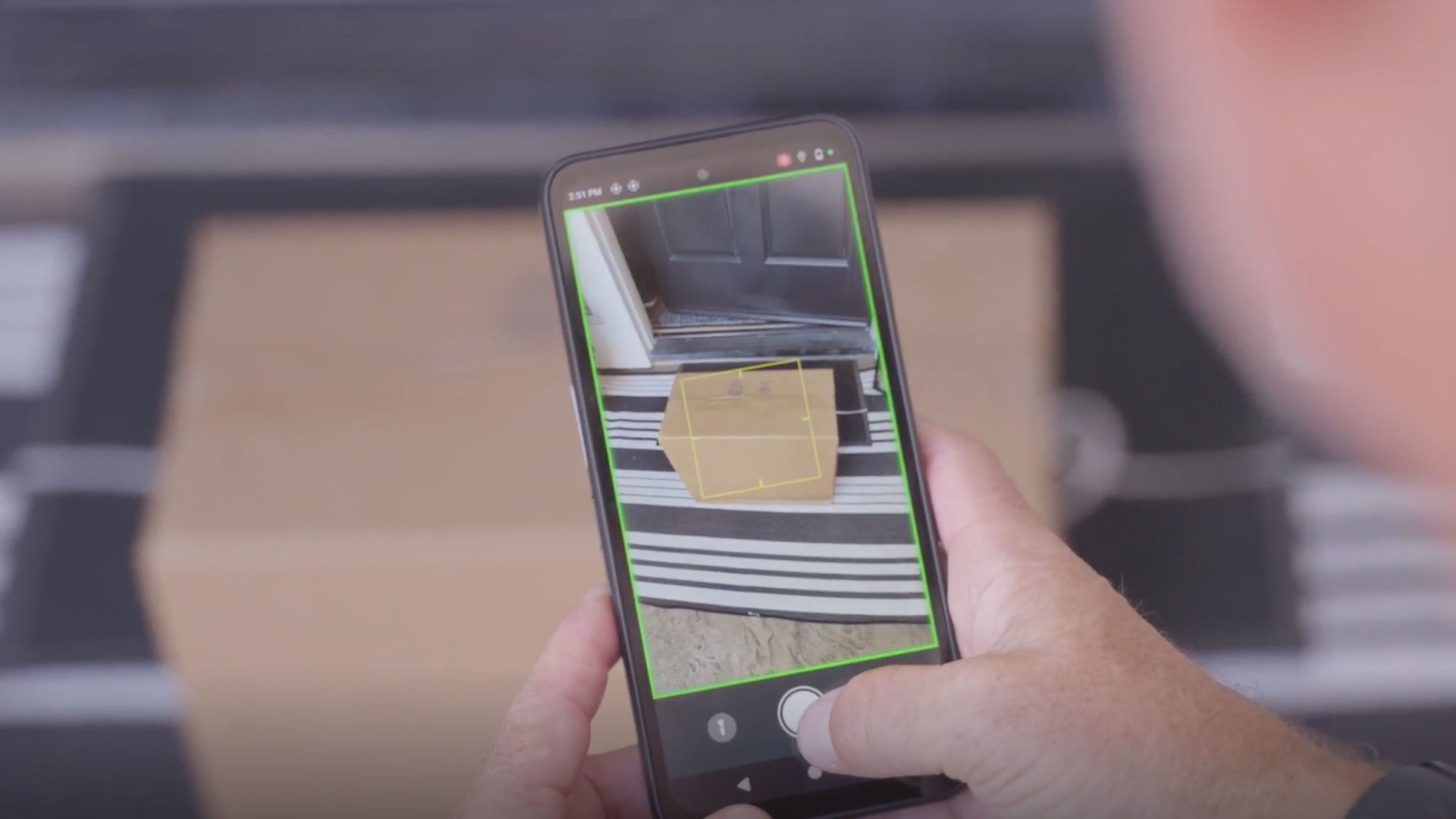
Then, when it’s time to head out, you can quickly make the necessary stop(s) to retrieve equipment, medications, and supplies for the day’s caseload. Since you now have a tablet loaded with software that can reconcile patient treatment plans with inventory needs and digitally generate a list – or automatically place the order with the right vendor/department – all you may have to do is walk into the building and grab your order. Even if you do have to do a little “shopping” in the storage room or stop in at the pharmacy, you can use the tablet’s built-in barcode scanner (yes, that’s a thing) to verify you’ve grabbed the right items and medications.
Once everything is loaded up, you can use the navigation app on the tablet to head to your first patient’s home, maybe even arriving early since the supplies pickup went smoother than usual.
Once you get unpacked, you quickly check the patient’s vitals (dropping the latest numbers into the tablet either manually or via a device-to-device plug-in using the I/O port), take some photos of any incisions, wounds or injuries that need to be notated in the file, then retrieve the detailed plan for medication administration, physical therapy, infusion, etc. from their electronic medical record (EMR).
If you administer medication or an infusion, you can use the barcode scanner again to ensure you’ve grabbed the right item and update the patient records with administration details, including time, drug, and dosing information. If you need to make other notes in the patient record, you can do so on the spot so that you don’t forget details later. There are removable keyboards that can attach to the tablet for easy data entry when needed.
Once you wrap up with your first patient, you can head to the car and quickly type in the address for the next patient, following the navigation to get to your next patient as efficiently as possible and enjoying a little bit of mental reprieve. Since you already updated the first patient’s record at the bedside, you don’t have to try to remember/recall anything throughout the day. Your mind is free and clear, and you’re confident the patient will receive the right care the next time since you were able to update other caregivers in real time about the patient’s status and recommended best next steps.
Now, if your days looked like this one, my guess would be that you would feel more satisfied with the work you put out and the care you give your patients. Thankfully, with the advancements in healthcare technology, this day could soon be your reality.
You just need to get set up with a single mobile device (ideally a tablet) that runs the right home healthcare-specific software.
What makes it “right”?
Well, you should only be using devices made of medical-grade plastics because you need to be able to disinfect the device often – between each patient, at a minimum – without damaging the device. If the device you’re using around a patient isn’t encased with these special plastics, which are the only ones that can be properly and repeatedly disinfected, then you’re potentially exposing your patients, their other caregivers and yourself to harmful pathogens that are readily spread via surfaces. So, that will whittle down your device options quite a bit.
In addition to choosing the right type of tablet, you need to ensure it has the right features and functionality. For example, you should be able to securely access patient records and connected medical devices/monitoring devices. In addition, the device should reliably connect to cellular and Wi-Fi networks (and stay connected) as you move from one place to the next, without you having to manually intervene to switch to the strongest network. And communicating with other care team members should be as simple as “push-to-talk,” a video call, or a quick IM if you do need clarity on treatment plans or a virtual consult based on a new development. There may be other capabilities you need based on the kind of care you provide (i.e., hospice vs. physical therapy). However, these are the basics.
I know you may not want to go through the hassle of switching out devices, getting new software set up, etc., but by doing so, you will likely spend far less time on secondary/administrative tasks and more time with your patients – where it matters most. Plus, the type of setup I’m talking about won’t fall solely on you (assuming you work for someone else) because the tablet and other components will be company owned/managed.
Now, if you’re self-employed – or the boss – then you may have to work a little bit with IT and other teams to make sure you’re buying the right tablet, that it can run the software specific to home health use, and that it’s configured properly from a security, wireless connectivity and access (SSO) perspective. But, again, it’s not something you’ll have to manage alone. In fact, depending on which device manufacturer and software vendor(s) you work with, you’ll probably have access to their solution engineer and IT support teams, too, which I know many smaller home health providers appreciate since they typically don’t staff large IT teams or even in-house IT teams.
More Reasons to Reconsider Your Current Tech Choices
I remember when the hospital-at-home model first started taking off. It was common to see clinicians practicing with consumer devices that offer basic capabilities like phone calls, GPS routing, and medical record logging. Some even had multiple devices to serve different purposes; a phone to call, a laptop to document and a tablet for medical records. But it doesn’t have to be that hard; it never did.
A multifunctional tech solution (such as a tablet with built-in voice calling, video, and scanning capabilities and a connected mobile printer) can give you the full “mobile office” setup you need to do all your work before you get home. That way, you have time to decompress after your last patient. A multifunctional device can also become the centralized location for all your data and medical records to be stored and located so you no longer have to jump from device to device trying to find patient information or charting with pen and paper for later input into a PC. Besides reducing the risk of forgetting what you needed to add to the record or relay to the patient’s referring physician, having real-time charting and communication capabilities helps protect the patient. You’re less likely to make a mistake inputting information when the info is fresh or automatically entered into the EMR.
Now, I want to note that while not all home health mobile computing solutions may be configured the same way, I wouldn’t consider a mobile device appropriate for home health use unless it comes with high-definition camera and scanning capabilities, the proper radios and high-quality wireless network connectivity capabilities to support virtual consults with other nurses and doctors, information retrieval/sharing and more. Of course, you need healthcare-grade security/privacy tools and access controls, too.
Something else to consider: if a patient has a crisis during your visit, time is of the essence. If you have to make a phone call – actually push buttons to input a number – that wastes time. So, I strongly suggest that you look for a healthcare-grade tablet or handheld mobile computer that has a dedicated duress button. That way, all you have to do is press that one button in case of emergency and your location will be marked and emergency services will be called discreetly.
Speaking of duress…if you’ve ever dropped your personal smartphone or tablet or spilled liquid on or around it, you know the panic that ensues. “Does it still work?!” That’s probably the first thought racing through your mind. Well, if you’re using the “right” mobile solution for home healthcare, that thought won’t cross your mind because you’ll know that your tablet or mobile computer can handle drops, spills, exposure to bodily fluids or chemicals (including disinfecting chemicals), and even UV light. It's not unheard of for blood to get on a device when a clinician is changing a patient’s wound dressing. And UV light is becoming more commonly used to disinfect devices. Well, both can be harmful to consumer-grade devices (i.e., the personal device you’re trying to use for patient care). Healthcare-grade devices, on the other hand, are built to handle it all without flinching.
A final consideration: if you work with patients who have vision deterioration but will need to see something on your device screen – perhaps lab results, imaging or even another healthcare provider doing a remote consult – having a larger-screen tablet on hand will improve their experience tremendously. If you work with patients with mobility issues, or you just want to carry the tablet around more comfortably, you can also add a hand strap made of healthcare-grade plastics that can be disinfected as intensively as the healthcare-grade tablet.
Where to Start
If this is a lot to process, I get it. I work in technology and know how much goes into making sure the right features and capabilities are built into devices – and making sure the right software is running on devices and connecting to critical information systems. If you’re a sole practitioner or a small business owner, you may feel like this is too much. But the reality is that getting you and your team equipped with the right mobile technology tools is no different than getting the right billing system online. You just need to find a technology partner that will work with you – and for you – rather than just sell you products and leave you to figure out how to connect the dots.
And if you work for a larger healthcare system and don’t feel this is your call, know you have more influence than you think. Tell your manager and your IT team what’s working and what’s not. Ask them to look into what I just described. My colleagues and I will be happy to talk with you all at once – even meet at your convenience – to show you the differences between the technology you’re using today and the technology you should be using for home health. Just give us a call.
Putting the Patient First
I know I started off this conversation talking about why you should reconsider the technology tools you’re using (or not using) to support your mental, physical, and emotional well-being as a home health provider – to become more efficient and organized. However, the technology you decide to use (or not use) isn’t just impacting you. It’s also impacting your patients’ physical, mental, and emotional well-being.
When you have easier access to patient information, such as medical records, you are providing a safer and more trustworthy experience for your patients. When you have faster access to patient information, you can answer all their questions versus being the one asking all the questions. No one likes repeating their medical history every time they see a new healthcare provider. People avoid getting proper care for that reason. They feel like they’re going in circles. They just want someone to come in and know what to do to help them feel better. Plus, some people can’t remember their medical history, which leaves them frustrated. So, knowing everything there is to know about a patient before you walk in the door the first time goes a long way to creating a positive experience for all.
Plus, when you can focus on patient care (versus wasting time on patient inquiries), you can get in and out in a timely manner and see more patients in a day if that’s what’s needed.
In other words, if you do nothing else today, acknowledge what frustrates you most about every other day – and what patients seem to complain about often. Then pick up the phone and call me or my colleagues to share what it is that you wish was less painful. We can then see if there’s a technology solution for each of those pain points – and if most (or all) can be addressed with a single technology solution.
###
Related Reads

Rikki Jennings, BSN, RN, CPN
Rikki Jennings, BSN, RN, CPN is currently the Chief Nursing Informatics Officer (CNIO) at Zebra Technologies where she is responsible for combining her knowledge of patient care, informatics concepts, and change management to effectively address the information and knowledge needs of healthcare professionals and patients to promote safe, effective, and efficient use of IT in clinical settings. She also serves as the strategic liaison for health IT efforts representing nursing and clinician needs.
Early in her nursing career, Rikki recognized a disconnect between purchased technologies and the understanding of their intended value at the bedside by her fellow clinicians and pursued Nursing Informatics. She is passionate about the utilization of technology to support safer, more effective care models. Over the past several years, her work in the healthcare IT industry has provided her an in-depth knowledge of the workflows and utilization of clinical technologies including clinical communication systems, bedside technology solutions, and data analytics tools in hospitals across the country. In 2019, Rikki was recognized in Crain’s Chicago Business’ Notable Women in Healthcare list. Rikki holds a Bachelor of Science in Nursing from University of Iowa.



![[Category, Subcat or Product] Representational Image 16:9](/content/dam/zebra_dam/global/zcom-web-production/web-production-photography/newsroom/2026-images/photography-web-newsroom-featured-03-16x9-en-us-013026.jpg.imgo.jpg)