Back to Basics: How to Use a Barcode to Automate Data Capture, Positive Patient ID and More in Healthcare Settings
Barcodes have been around nearly three-quarters of a century, and actively used in healthcare settings for over 50 years. So, as a longtime clinician and technologist, I’m always shocked when I visit hospitals and clinics and see staff still trying to manage every aspect of patient care manually.
Even in big cities with strong digital economies, doctors and nurses are still charting, labeling medications and creating patient wristbands with pen and paper. Yet, even in smaller or more rural healthcare systems situated in communities where technology penetration is low, nearly all patients and staff members have personal smartphones. It’s quite baffling.
What’s even more perplexing is that my colleagues and I have seen more extensive barcode technology utilization and workflow automation in field settings – pop-up clinics run by non-government organizations (NGOs) – than in some big hospitals across the Asia Pacific (APAC) region.
Why are some healthcare administrators hesitant to digitalize and automate data collection and workflows using the barcode – a proven, familiar, mature and simple technology? And why are healthcare systems in Vietnam, Thailand and Indonesia still in Stage 0-Stage 4 of the HIMSS Electronic Medical Record Adoption Model (EMRAM) while healthcare systems in Singapore are between Stages 6 and 7 and implementing RFID technology to track, trace and locate everything from medical supplies and medications to patients and staff?
We knew over 20 years ago that fundamental data digitization and automated data capture could dramatically improve patient care and, thus, influence more positive outcomes:
A 2005 study published in Patient Safety and Quality Healthcare found that implementing barcode technology in five units of a community hospital reduced errors by 82%!
A different 2010 study published in the New England Journal of Medicine in the U.S. confirmed that barcoding technology was preventing 90,000 serious medical errors every year and reducing mortality by 20%!
So, this shouldn’t be a matter of mistrust in the technology. Yet, as I have met with clinicians across APAC in recent months and years, I’ve come to appreciate the need for education about:
What the barcode is and what it can do.
Why the barcode is the easiest way to build confidence in care among patients and clinicians.
I have spoken with nurses who were hesitant for their hospitals to use barcoded wristbands because they typically see barcodes on “cheese at the store.” They couldn’t fathom the same technology being used in a clinical setting. (True story.)
After I explained the versatility of the barcode to them across different applications and how specifically it could be used to help people – both them and their patients – in healthcare settings, they started to be more open to the idea. They acknowledged how risky it is to have to positively identify patients and correlate the correct medications using handwritten information on a wristband that often is not legible. They don’t want to be held liable for a mistake due to a misinterpretation of someone’s writing, nor do they want to delay patient care trying to figure out what the wristband or chart say.
Once they started to verbalize the issues they had essentially normalized for decades, then they started asking questions about what was possible, and I began by highlighting the Scan4Safety program in the UK (as I do every time I speak with someone about how to move from manual to digital processes.) Scan4Safety has become a poster child for proper operational productivity, supply chain management and patient safety techniques over the last several years. That’s because the National Health Service (NHS) has focused on implementing technologies, creating new digital information flows, and setting standards that make it easy for clinicians and other staff to confirm the action they’re taking is in line with the “right patient,” “right product,” “right place,” and/or “right process.” They have proven how end-to-end operations and entire healthcare experiences can be transformed using the barcode. Not RFID. Not robots. Not AI. But barcodes.
If you’re based in a country that’s more technologically advanced, where RFID, robots and AI are becoming commonplace in healthcare operations, you might be thinking, “Healthcare is way beyond the barcode. The business case has been proven, the technology’s use is standard, and we need to be looking at how we can build upon barcode systems to further automate data capture, workflows and decision-making for the sake of our people.” And you would be right on that last part. The value proposition for barcode systems has been proven time and again for everything from positive patient identification (PPID) and medication administration to Unique Device Identification (UDI) data collection/utilization and regulatory compliance. It is used every day for the track and trace of pharmaceuticals, medical devices and patient care. However, the healthcare community is not moving “beyond the barcode.” It’s building upon it by finding new ways to leverage the systems already in place and the data being collected with every scan.
We haven’t even begun to scratch the surface when it comes to how many different ways barcode data can be aggregated, sliced and diced to inform care decisions, build confidence in care actions, and improve the accuracy and timeliness of billing. The barcode can even help increase healthcare accessibility by expanding clinician availability and facilitating faster patient turnover. Every minute saved by not having to figure out what someone wrote on a wristband or chart is a minute faster that a patient can get proper care and go home, making room for another patient to be seen. My peers at Zebra and in the healthcare community have talked quite a lot about how the barcode could be beneficial, so I’ll refer you to these conversations for follow-on learning to come back to after reading this blog post:
COVID-19 Just Reminded Us Why Modern Medicine Needs Modern Technology Tools
How Simple Patient Identification Tools Drive Better Front-line Care
Setting the Record Straight: Why Lab Technicians Rely So Much on Scanning Technology
Before you click away to hear what the others had to share, I want to call out a few best practices when it comes to barcode-based processes in healthcare (especially PPID and medication administration verifications):
1. Don’t Just Set Policies. Teach Them. Enforce Them. Adapt Them.
Though many people like to consider technology a solution to nearly every modern problem, the reality is that technology can’t completely account for human behavior. For example, recent observational studies in healthcare systems around the world show that barcode technology can effectively reduce errors in medication administration if – and only if – staff are properly trained on how to use the technology and comply with processes designed to ensure technology effectiveness. If there is any deviation from the policy or process, errors can occur.
In one study conducted in Norway, researchers watched 44 nurses administer 884 medications to 213 patients. As reported, “There were barcode medication administration (BCMA) policy deviations for more than half of the observations, with task-related policy deviations occurring with 66% of patients during dispensing and 71% of patients during administration. Organizational deviations included failure to scan 29% of medications and 20% of patient’s wristbands. Policy deviations also arose due to technological factors (e.g., low laptop battery, system freezing), as well as environmental factors (e.g., medication room location, patient drawer size). Most deviations were caused by policies that interfere with proper and safe BCMA use and suboptimal technology design.”
What this tells me is that a few different things could have been happening. Staff may not have understood the policies or taken them seriously. Or perhaps they didn’t understand how to use the technology, so they reverted to what felt easier to them, even if it required more effort or introduced more risk. Alternatively, the policies may not have aligned with clinical best practices, so they deferred to what they felt was the better move. In any case, you must assume all could happen in your facilities when barcode technology (or any technology) is in play. So, form a team of inside consultants to help ensure you’re:
setting the right policies.
designing the technology stack to support those policies and other operational policies/healthcare standards in full.
doing enough to make staff feel comfortable using the technology.
There’s going to be a learning curve, but there is a lot to be learned from others who have preceded you on this digital transformation. If you’d ever like to talk to Zebra customers about their approach to barcode-based automation (data capture, decision making, verifications, etc.), reach out to your local Zebra representative or me. We can arrange for you to hear how they designed their systems and why they chose that design, how they involved others (including IT, finance, clinicians, etc.) and how they use continuous feedback loops to expand and build upon their barcode systems.
2. Don’t Hesitate to Bring in Outside Help.
I know that you know your people best. You also know your policies and systems best. But how well do you really understand barcode technology systems, how they need to be integrated into other systems, how to manage them, and how to scale them? Too many healthcare IT administrators try to handle everything in house. But they aren’t barcode system engineers. Just like you wouldn’t want an unlicensed nurse providing care, trust me when I say you don’t want an unpracticed team member spearheading a project of this magnitude. Though barcode technology is pretty straightforward to use, there are lots of special considerations that must be made with each implementation. It’s not a one-size-fits-all, plug and play solution. So, please bring in the right people (including third-party engineers and consultants) to help advise on the project, even if you do the work and they’re just steering you in the right direction and making sure you see all potential obstacles (and avoid them).
3. Do Consider All Possible Barcode Applications, Not Just the Obvious Ones.
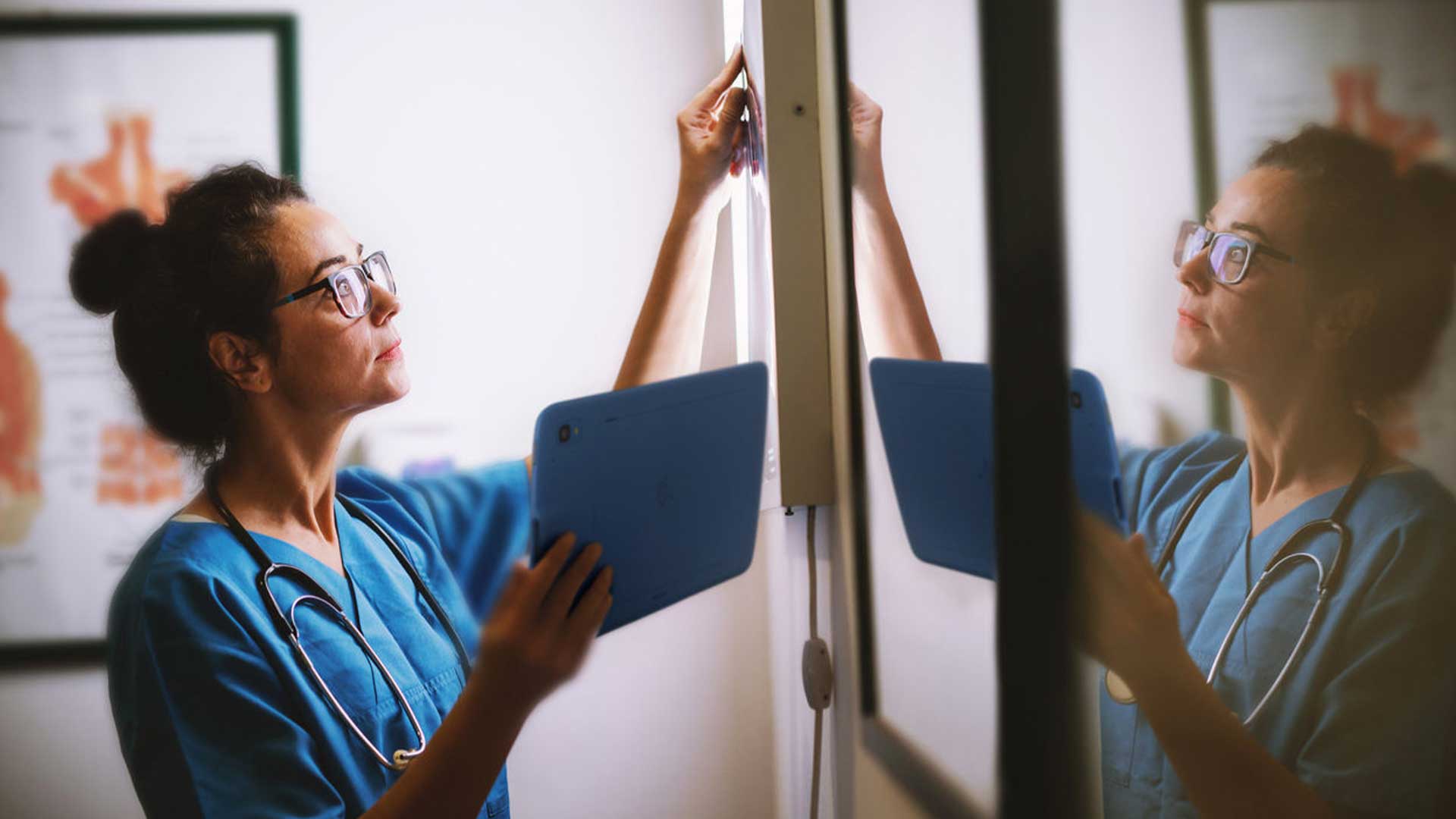
Configuring barcode scanning systems to support PPID and medication administration should be your first priority, followed quickly by UDI. But think about how you can leverage the barcode to collect data related to lab specimens, pharmaceutical stock, staff attendance or even blood distribution. For example, The Royal Children’s Hospital found that using barcode systems to accurately scan blood products tremendously improved patient safety. Calderdale and Huddersfield NHS Foundation Trust clinicians are now using mobile computers with built-in barcode scanners to help document patient data in real time at the bedside. And those responsible for transporting specimens at QE Facilities feel good that they are bringing the right samples to the right place, that they’ve recorded the collections and deliveries properly, and that they can move the samples as efficiently as possible to help shorten results turnaround times. Think about how a barcode scan can affect billing, operation room turnover time, and more. Once the right system is in place, you’ll be able to scale as needed. But you must get the right system in place.
That said, I know the barcode is not the end all, be all for healthcare. But it is the foundation for everything else you need or want to do to earn the trust of patients, loyalty of staff and praise from your superiors and regulators. To quote a paper recently published in an academic journal:
“We now have international standards for barcodes and for healthcare organizations. Barcode technology is not the sole answer to the challenge of supply control and patient safety. However, it is a tool that, within a culture of safety, can help to increase clinical and patient trust in the system processes. Together with proactive management of risk, HFE, and the building of resilience, it can help to build a safer and more efficient healthcare system.”
If you need help selling key stakeholders on the benefit of the barcode, let’s talk. I can share some resources that will help you get their buy in and ease the change management process with clinicians specifically. In the meantime, I encourage you to read these two articles:
Why You May Want to Reconsider How You’re Handling The Five Rights to Medication Administration and Medication in General

Johnny Ong
Johnny Ong has been on the front lines of healthcare for over 20 years. He currently advises healthcare administrators and clinicians on best practices for clinical workflows, automation and more as the Healthcare Practice Lead for Zebra in APAC.