What Can Hospital Leaders Do to Accelerate Digitalisation and Meet New Efficiency Mandates?
I'm very lucky in that my hospital experiences have been limited to a broken arm as a youth, a handful of babies and a few visits to recovering relatives. So, now that I’m a healthcare solutions marketer, I wanted to deepen my experience of healthcare. I wanted to learn at a practical level what hospital administrators, clinicians and support staff must do to deliver the excellent care we all expect as patients and for loved ones, so I took the plunge and signed up as a volunteer at my local hospital. Not a simple task may I add. The screening process was as thorough as if I were applying to MI5! But I persevered and I now give back Friday afternoons to help elderly patients in a ward with an average age of around 90 years old. I make tea, fetch tissues, and play Scrabble, but the best bit is having conversations with the most incredible people about lives well lived, family present and gone.
And whilst all this wonderfulness is going on, I'm absorbing by osmosis the goings on in a typical UK hospital. I see the level of care patients receive, which is everyone’s top priority, the collaboration between teams, and a level of empathy delivered with a ‘chin up’ attitude that keeps patient spirits high at what can be quite worrying times.
So with this new, insider experience, it was from an enlightened perspective that I read through the UK government's ‘2023 Mandate to NHS England’ and considered how it would impact the ward and world I had now become a light part of. I was curious how the drivers from on high would positively influence the patients, people and processes I had become immersed in on the ground. Specifically, I wanted to know what actions administrators, clinicians and even volunteers like myself would need to take to meet the government mandate objectives for the NHS in 2023. How were we collectively supposed to:
- cut NHS waiting lists and recover performance?
support the workforce through training, retention and modernising the way staff work?
deliver recovery through the use of data and technology?
Just as importantly, how would we measure progress against these objectives?
The NHS, like most health organisations around the world, is under pressure from a growing and aging population, rising prevalence of chronic diseases and workforce shortages. Its patients are influenced by the wider digital world and expect greater transparency into their care options and the care actions taken, along with more convenient care options and greater access to healthcare providers, medications and other supportive resource. We are also not yet fully over the impact of the pandemic, with waiting times to see a healthcare provider remaining stubbornly high.
In light of this, the UK government has provided an extra £14.1bn to help cut the queues, whilst acknowledging that digitalisation is the key to securing the future safety of the NHS, stating that 'digitally mature trusts operate with approximately 10% improved efficiency compared with their less digitally mature peers.'
In short, digitalisation done correctly bolsters efficiency and improves patient care.
So, what did I experience on the 'street' and could digitalisation offer any obvious solutions?
Patients Have Lots of People Caring for Them – And Lots of Questions About Their Care
One thing I noticed during an extremely long, high scoring and thoroughly competitive game of Scrabble with 94-year-old Dorothy was just how many staff attended to patients. During our match, we were visited by seven different people! A nurse checked blood pressures, carers helped wash a nearby patient, a cleaner swept, the head nurse gave good news that a care agreement had been accepted, a junior doctor explained what cellulitis is, a consultant explained some tests, and a maintenance engineer read the RFID tags on some medical equipment.
What struck me was the amount of people and how they seemed to disappear into thin air. Kathleen was in the bed next to Dorothy and forgot to ask the consultant when she could go home. Sensing her distress, I raced down the corridor and managed to find a junior doctor who came back to explain her test results would determine next steps (i.e., if she could go home). Understanding made the scenario easier for her.
It was lucky I was there, in sensible shoes and in triathlon mode!! The consultant had vanished, and if I'd left it much longer the junior doctor would have evaporated into the hospital ether too. Without me, and without an explanation, it would have been a worrying few hours for Kathleen.
But imagine if the consultant could be found instantly (without someone like me physically chasing them down). Location solutions exist. This capability to find a staff member instantly without having to physically search for them is tried and tested. In a fully digitalised world, anyone on the nursing team could look at a tablet or a mobile computer (that looks and feels like a smartphone) to instantly locate people or assets. If our consultant doctor wore an RFID wristband or badge and the hospital was set up with antennas at all doorways, then a simple glance at a digital handheld device screen like a tablet or mobile computer would indicate what room he was in. If he was still on my ward, I could nip over and relay the question. Or if he’d moved on to another building, I could send a secure message using an app built for instant staff communication to his clinical mobile device. He could even respond via a live telehealth video chat through his device if he wanted to have a ‘face to face’ with Kathleen or me.
And that slicker system, with more patient throughput, could only be good for outcomes.
Healthcare Staff Have Lots of Questions Too – About Patients, Best Practices, and More
The second priority of the UK government’s mandate that NHS ‘support the workforce through training, retention and modernising the way staff work’ can be influenced by digitalisation. Simply reducing the burden of administrative tasks can enable clinicians to give back more time to patients – what many signed up for – bolstering moral and supporting retention. Training can be done remotely and efficiently via mobile computing devices to keep skill levels current and high. Similar technology can also be harnessed to positively identify patients and link them safely to timely treatment plans, reducing errors and staff anxiety.
My colleagues (many of whom are practicing clinicians) have spoken extensively about some of those technologies, so you’ll want to see what they’ve learned about which technologies can solve multiple problems quite quickly:
Why You May Want to Reconsider How You’re Handling the Five Rights to Medication Administration and Medication in General
However, The Answers Can’t (or Shouldn’t Be) Found in a Stack of Paper
The final mandate objective is to ‘deliver recovery through the use of data and technology’. This is where the government clearly identifies how critical data digitisation – and the subsequent digitalisation of information flows – is for the long-term sustainability of the NHS. Artificial intelligence (AI), which is used in the latest screening techniques to detect illness sooner, and equipment that allows more people to be treated at home were called out specifically.
In my digitally native world, it seems somewhat alien to realise that medical records remain paper based in many areas, with targets that ‘90% of NHS trusts and foundation trusts should have electronic health records by December 2023, and 95% by March 2025, and 80% of 12 Care Quality Commission (CQC) registered adult social care providers should have digital social care records in place by March 2024.’
I was really quite surprised by the amount of paperwork I witnessed whilst volunteering. Medical records were still being made on paper, which I did not expect operating from my almost paper free life. In fact, a recent declutter of my loft saw me reduce down from close to 50 folders to a manageable two – house purchase docs and academic certificates – and work-wise my life is purely electronic. Having all the records electronically would mean my consultant could access all the information required to advise the patient, from a separate building or maybe even offsite, hugely increasing efficiency and likely increasing the amount of patients he could see, all driving down the never-ending waiting lists. Simple steps to cut NHS waiting lists and recover performance.
We Must Eliminate the Gray Areas and Guesswork Still Common in Healthcare
I found it encouraging to see in the mandate that 'By March 2024, all trusts should adopt barcode scanning of high-risk medical devices and submission to the national, mandatory Medical Device Outcome Registry.' High risk items include powered implants or partial implants left in the human body such as implantable cardiac pacemakers and defibrillators. As per the NHS Scan for Safety program, scanning is cost effective and improves patient safety through:
Generating early warning systems for expired medical devices.
Fast and efficient retrieval and recall.
Monitoring implanted devices on a patient’s Electronic Patient Record (EPR).
Freeing staff from manual data entry and improving accuracy.
The registry will be used to improve patient safety and outcomes in procedures that use high risk medical devices.
Fortunately, barcode scanning was quite a common element of my volunteering via barcoded wristbands on all the patients I saw. This identification could link patients to their EPR and provide a permanent paper trail for any treatment, procedures or drugs, even as consultants and doctors change.
Related Read:
Yet the paper-based medical records posed a weak link in the patient journey I witnessed, one that could be solved by an element of more advanced digitalisation that I noted as Dorothy put together yet another a treble word score and I considered where to put my Q.
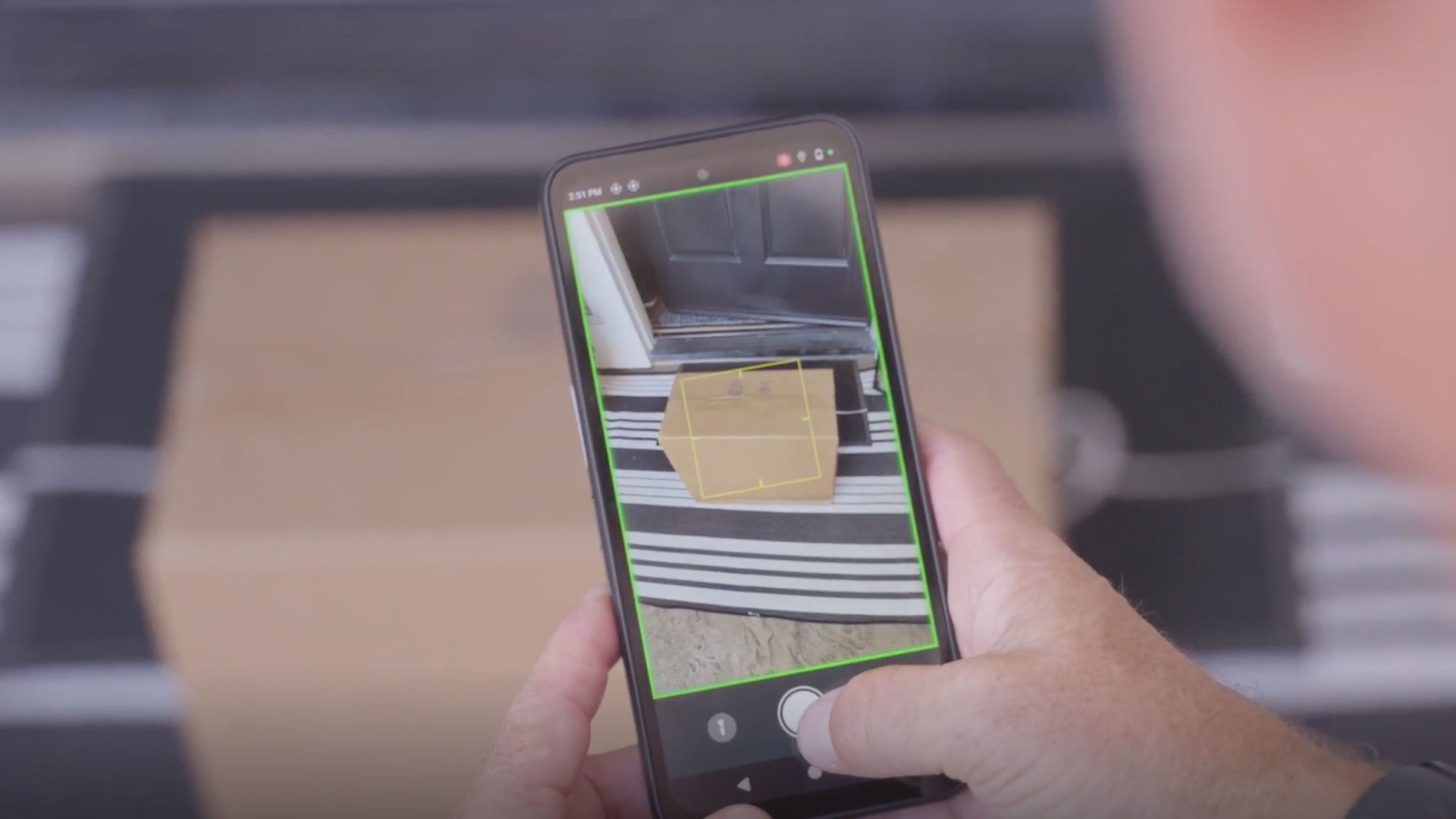
The maintenance engineer politely introduced himself then waved an RFID reader around various pieces of medical equipment surrounding Dorothy's bed undertaking a stock take. This level of asset tracking really can drive efficiency as you know where every asset is, so there's no need to spend time looking for things or unnecessarily purchasing replacement items. Or, if they're rented items like some barometric beds, it ensures they never fall out of contract, enabling you to evade extra costs. However, not all facilities are using RFID for asset tracking, and those that are may be missing out on opportunities to use it more extensively.
The next step up from a handheld RFID reader to account for certain high-value equipment is to implement fixed RFID readers around the hospital. Then you’ll have a ‘last known location’ of every item you tag, which could be everything from wheelchairs to blood bags, pill bottles and even trays. There’s location-tracking software that can sync with the readers to aggregate all the location data being captured and provide a digital view of your entire hospital’s status, at least in terms of asset positioning. But it offers more than a static view. It can help keep things moving. In a recent use case with surgical tray sterilisation, hospital staff found RFID to greatly improve asset availability and workflow efficiency. And as we both know, time and money saved via a streamlined system opens up more appointments and drives down queues.
Making the Right Connections – Between People and Machines
Whilst figuring out how to make the patient experience better right now, it's also very important to think to the future. As hospital operations become increasingly digitalised, it becomes ever more important to have wireless networks that can handle the load from robots, sensors, location solutions, and other connected IOT and AI-based technologies.
Think about the load that’s increasingly being placed on networks…
A continuous flow of vital signs from patients located in a multitude of locations, combining with statistics to predict outcomes and deliver tailored care plans.
Robots undertaking neurosurgery guided by a surgeon on a different continent – and taking patient temperatures, triaging and delivering food.
Telehealth consultations during virtual surgeries, with added data input from wearables relaying patient vital signs to people inside and outside the operating room in real time.
Wearables guiding physiotherapy programs, alerting care providers to patient falls, and keeping chronic patients like diabetics well for longer with personalised programs.
The instant locationing of every asset and person.
Think about what will happen if we keep placing that demand on Wi-Fi networks – networks that are overloaded simply by a growing number of connected smartphones, clinical mobile computers and tablets. We can’t put all our eggs in one basket. Ideally, everyone in healthcare should be talking about 5G and what it’s going to take to get healthcare operational and information technology systems migrated to 5G networks inside and outside the four walls.
With speeds 100 times faster than 4G and ultra-low latency, 5G has the ability to handle many more connections without faltering. 5G is imperative for the volume and sensitivity of new healthcare – an enabler and catalyst for better outcomes.
I know you might think I’m ‘ahead of the times’ on this one considering many parts of the world are still on 3G or not yet able to access 5G networks. Plus, healthcare leaders have spent a fortune on Wi-Fi infrastructure that no one wants to rip and replace. But I’m not saying 5G is an urgent action item – just an urgent topic of discussion. If anything, you should be asking technology providers about what it will take to get a private wireless network online in general. Whether it’s 4G or 5G right now really doesn’t matter because cellular connectivity offers many advantages over Wi-Fi when it comes to network stability, predictability and even security (which patients will be keen on with EPR use rising). Standing up a cellular network that you can fully control within your facilities is going to be table stakes sooner than you think. And you won’t have to ‘replace’ anything as it will work alongside your Wi-Fi networks. The Wi-Fi could be reserved for patient/guest use while private wireless network access could be prioritized for staff communications, telehealth, robotic surgeries, virtual wards, patient monitoring and more.
My Recommendation from the Front Lines
So, what do I conclude from my work on the wards?
The patient care I witnessed was wonderful, and the processes worked. Old school paper-based records sat alongside advanced RFID-based inventory management. The pen worked as hard as the barcode but was intrinsically less reliable. Everyone was ready to help, but they didn't always have the tools to provide the answers. My ward was full, and everyone was calm and relaxed with an excellent standard of care.
But (there’s always a ‘but’) with digital reporting, location data and tools to communicate from disparate locations, the system could perhaps be a bit more efficient. A 10% efficiency gain would mean more patients treated, Dorothy and Kathleen getting home that little bit quicker, and waiting lists reduced. Patients might also feel more at ease while there, as would staff since asking questions and getting answers would be more of a stationary task than something that looks like marathon training.
A happy, healthier solution for all.
###
Curious How Clinicians Feel About These Technologies?
Here’s what they have to say…
What Is It Going to Take to Deliver the Right Patient Care at the Right Time Every Time? These Nurses Have Some Ideas.

Lorna Hopkin
Lorna Hopkin is Product Marketing Advisor at Zebra Technologies with responsibility for Zebra healthcare solutions and advanced location technologies. Lorna joined Zebra in August 2018 as part of its acquisition of rugged tablet specialist Xplore Technologies.
Lorna is a chartered marketer and has two and half decades’ experience across a wide range of industries. At Zebra, she has launched a variety of products into the healthcare space and other verticals.
Lorna is a tireless advocate for health and fitness at Zebra and in her spare time participates in Ironman competitions and enjoys writing about her experiences at https://theordinaryironman.com/